I fondly remember 5 years ago when I came to Haiti with 4 other monsooners as we backpacked up from the capital city of Port-au-Prince to Cap-Haitien and gazed out from one of the most beautiful fortresses of colonial America.
I had a great crew to travel with back then.
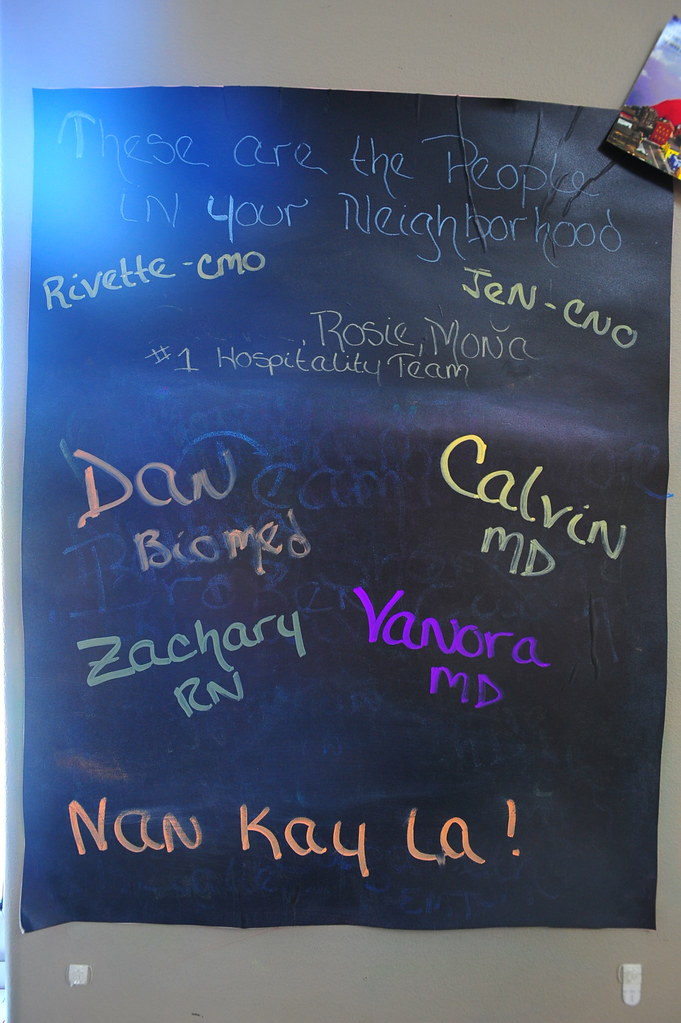
And I have a great crew with me this week:
So I’ve returned to Haiti, this time with my fellow colleague and former nurse at Jacobi, Zach, to volunteer here for a week at Hospital Bernard Mevs, the only hospital with critical care capabilities for the capital city of Port-Au-Prince. We’re also joined by Vanora, a wound care expert who just recently graduated from medical school and is applying for a residency in Family Medicine. The efforts are through the non-profit and Florida-based Project Medishare, and one of the few organizations that promote sustainability in international disaster and critical care relief that I know of.
To work at their main hospital site, their resources allows them to accept only licensed medical professionals above a certain training level (so for residents, they take PGY-3 and above) who not only are capable of handling a critical medical situation during the first few golden minutes of resuscitation on their own, but also be able to teach — as well as have the humility to learn from — the local Haitian medical staff. And after speaking with my colleague and co-resident Dr. Shazia Rahman who volunteered here just last year, the only way I could know for sure if this would be a good fit for me was to try it out.
Either way, it’s good to be back.
Upon arrival at Port-au-Prince (PAP) airport via a morning Jet Blue flight, we were picked up by our wonderful and superhuman Volunteer Coordinator Stacy, as well as our Haitian driver Philippe outside the airport and taken directly to the hospital and our living quarters inside the hospital compound.
Our dorm beds were more comfortable than I expected and we were informed beforehand to bring our own sheets and pillows (although they do offer fitted sheets if you need them and the group is small enough). I brought a sleeping bag liner with my inflatable travel pillows that did just fine — slept like a baby 9 hours every night!
Right outside our dorm room is the kitchen and dining area where we spent most of our time after work hours.
And on our rooftop, we got great views of Port-au-prince and our surrounding neighborhood.
Hospital Bernard Mevs itself is a gated compound facility (armed guards and all) that has an emergency room, 2 general inpatient units, a spinal/neuro inpatient unit, a medical intensive care unit, a pediatric intensive care unit, a neonatal intensive care unit, a pediatrics inpatient unit, and a separate Pediatrics ER.
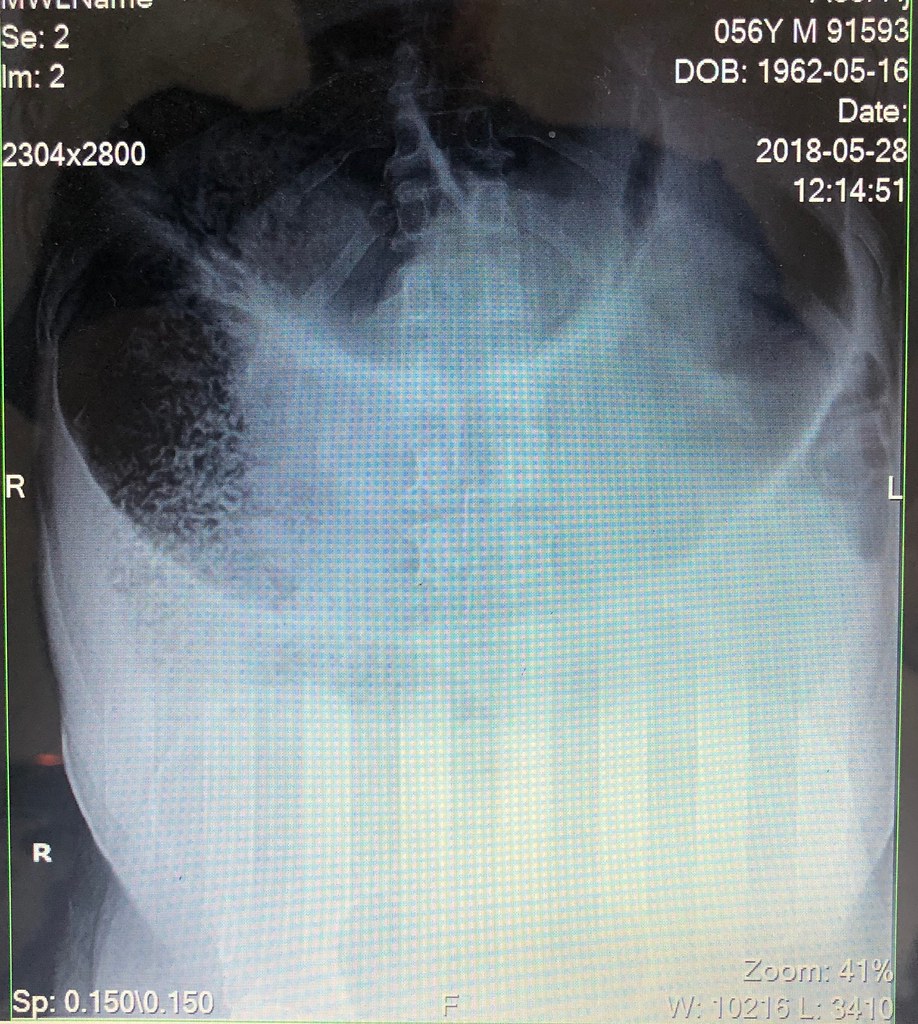
For diagnostics, they have their own mobile CT Scanner which sends its images back to the United States via a PACS-like system for official readings. Unfortunately for us it was down the entire week we were here, which made for some interesting management decisions for our fair share of elderly head trauma, gunshot victims through the abdomen and pelvis, aortic dissection, pulmonary embolisms…
They have a single x-ray machine which can be made portable if absolutely necessary. All X-ray films are read by the doctor ordering them (which means it was me this week…); there are no radiologists on site to give you any official readings (eek!).
They can do all basic labs except blood gases (they have I-STATS but not cartridges for them):
And while I chose not to photograph areas with patients such as the inpatient units and the Adult ER, I was lucky enough to see and take photos of empty pediatric units that are currently being renovated.
To give you an idea of what the Adult ER is like (and where I’ll be working for the next week), it’s about the same size as the Pediatric ER you see here (fits about 3 beds and 3 chairs):
In addition to the Pediatrics ER, they’re renovating their Pediatrics Intensive Care Unit:
And their neonatal intensive care unit:
This is the world outside our hospital:
Every night we drove up somewhere for dinner, including upmarket Petionville:
On our day off (usually every Friday) we got a morning tour of central Port-Au-Prince, seeing where the earthquake dealt the most damage:
We drove to the famous tourist staple Hotel Oloffson for lunch and beer, where I did the same thing 5 years ago:
Then it was a 40 minute drive up to Point De Vue (Observatoire), where we grabbed a beer and shisha overlooking all of Port-Au-Prince at The Lookout bar:
Afterwards we kicked back at Karibe Hotel for a spa massage and drinks by the pool. You can also head up to their rooftop bar Asu Rooftop Lounge for more upmarket drinks and dancing:
As for the actual medical volunteer work itself — I saved the best for last, but it’s also just in case some of you get queasy with the sight of blood and bodily fluids. You have been warned!
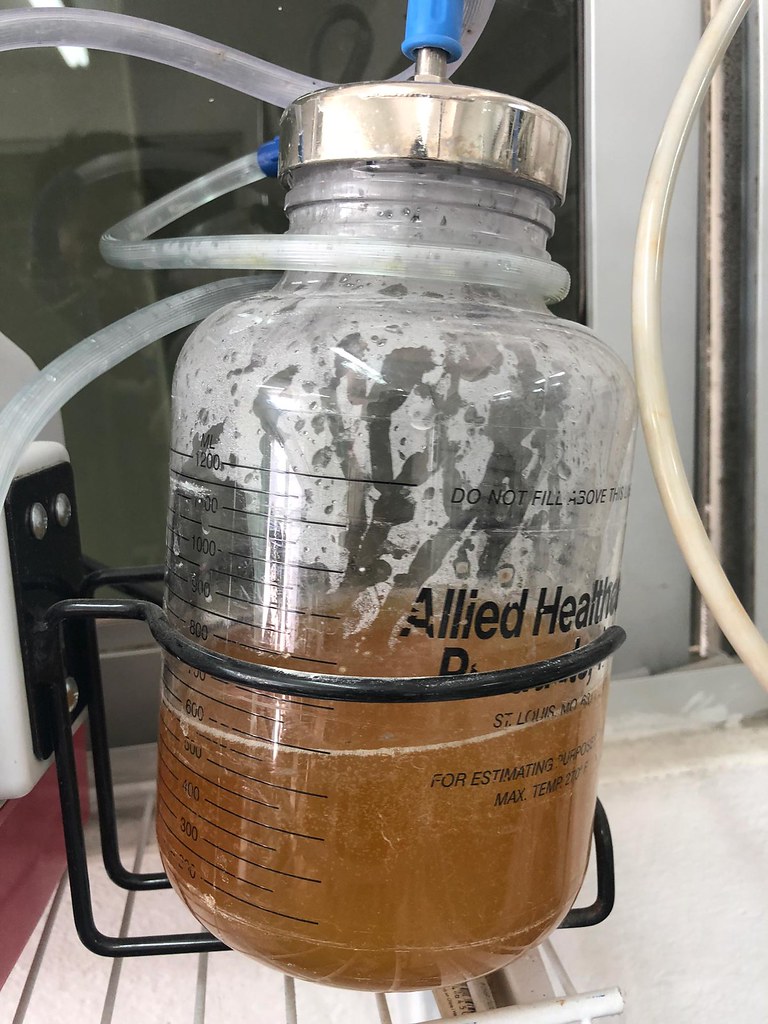
I started my week off putting in bilateral thoracentesis/pigtail chest tubes:
My second day took on 3 traumas: an electrocution, and 2 patients with gunshot wounds that arrived all at the same time. I had to make decisions on which patients I could send to the operating room based on our ultrasound findings since our CT Scanner was down:
My third involved an R/O thoracic aortic dissection with a widened mediastinum >8.5cm and a flap on my ultrasound of the thoracic and abdominal aorta — we had to send this guy out to an outside hospital for the CT (since ours was down all week). That was an ordeal to arrange.
I also got called in the middle of the night to work on multiple emergent cases in the Intensive Care Unit and the ER, so I would run down in nothing but my flip flops and pajamas (Shazia, you did warn me about this):
My fourth day involved intubating a SWAT police officer with a GCS of 7 that was found down at a crash site for an unknown amount of time at 2am in the morning. After intubating him I hopped in the ambulance to transport the patient to another hospital in Port-Au-Prince to get CT Scans, only to have a small argument with the technician to include the C-Spine after he initially refused to do any more than scan the head. We got both and transferred the patient back to our hospital for an ICU admission with neurosurgery.
And then my next and final day was ortho day where everyone came in with a significant OR-worthy fracture.
One had the largest “coffee bean” sign (aka volvulus) I’ve ever seen. I sent him straight to the OR.
Overall, this was a meaningful week where the most interesting cases weren’t necessarily the pathology, the clinical presentations or the acuity of our management, but rather the jiujitsu decision-making in more austere, resource-poor environments where I had to make calls regarding rationing care appropriately.
Although many of us think we’re all somewhat prepared for these kind of decisions after training at some of the rougher county programs in the United States, it’s very different when you’re actually put in the hot seat and making those decisions on your own. Yes, we may know what decisions to make, but do we know how and furthermore, are we comfortable with making them? Only actual experience such as this can give us the answers to those questions.
I truly am grateful for Project Medishare and Bernard Mevs Hospital for granting me the privilege to hit the ground running here and making these kind of decisions from minute one. You’ve instilled in me the humility of having to understand what goes on in the world of Emergency Medicine outside our bubbles and I cannot underestimate such an opportunity.
I also want to give a shout-out to Stacy, our coordinator, for going above and beyond to making sure all the volunteers were comfortable, safe, well-fed, well taken care of, loved, and entertained the entire time we were here. It was fitting we came during the middle of Mother’s Day celebrations in Haiti as you were like a mother to us all. Also big thanks to Jen, Sam, Raphael, Kency, Drs. Rivette (especially for the kind things you wrote!), Germain (for getting to hit the ground running on day 1), Gordon (for being the trauma magnet that you are!), Levequé (for letting me run the ER by myself for hours!), and Pontius (for being the best co-doctor to work with everyday!) for your kindness, professionalism, and warmth throughout this entire experience. There was never a bad moment and never an instance where I felt unsafe.
It has been a privilege to have worked with you all and I look forward to coming back soon. Much love.
Zach also had this to write:
Thank you so much to everyone that donated and made my trip to Haiti possible. I’m still processing all that I saw and experienced, but the trip was incredible, and I can honestly say that we made a difference.
We learned from the staff of Hospital Bernard Mevs and we shared with them our knowledge and experience as well. We worked on patients with spinal injuries, gunshot wounds, electrocutions, and congenital illnesses. We treated babies that were so malnourished, they required intensive care. We gave our blood, sweat and tears, and will be sure to return one day and do it all again.
Thank you again to Calvin D. Sun for organizing the trip, to the staff of Bernard Mevs . . . thank you so much.
![]()
- At time of posting in Port Au Prince, Haiti, it was 28 °C - Humidity: 69% | Wind Speed: 11km/hr | Cloud Cover: partly cloudy