A PSA on what “Plateau’ing” really means for us.
(TLDR: things seem to be calmer this week in the ER, but #dontfuckitup and #keepstayingthefuckhome)
![]()

That things are getting “better” is a relative statement: You put sugar on poop, it’s still poop — Forgive me if I’ve developed some trust issues nowadays when people claim any “future projections.”

1) “Plateau’ing” means if 100 new patients came in yesterday, another 100 patients comes in today (instead of 100 on day one, 120 on day two, 140 on day three, etc,).
Think about that among ERs that were originally built to safely fit 30-40 patients at a time, and that having up to 100 patients a day consecutively could still mean patients can no longer fit inside an ER and go into cardiac arrest in the waiting rooms (which I actually had last weekend)
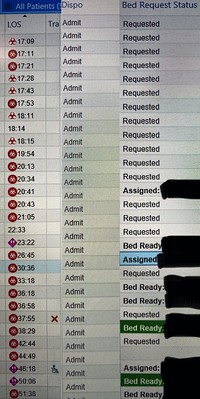
2) It takes about 7-12 days — and sometimes up to 20 days — for a COVID-19 patient (who was sick enough to be admitted to the hospital) to eventually recover. That means hospitals can keep getting fuller and fuller, even with a “plateau” of X patients coming to the ER everyday (of which an even higher than average % will still be admitted to the hospital due to COVID-19 being unusually associated with complications/sequelae such as embolic strokes and viral myocarditis)
3) What we need is a dip — not a plateau — that lasts long enough will allow us enough time to discharge enough patients (aka DECOMPRESS) from the ER and hospital, and accommodate the next wave of patients that come when we all break quarantine (whether it’s because we have a false sense of confidence, when the weather gets better, etc.).
Otherwise next month patients are not only going to die in the waiting room, but also on the street!
4) In other words, a cup pouring out at a steady plateau/rate will eventually run out of liquid, unless we slow the pour (aka a dip of patients coming to the ER) or we add to the cup (aka building new giant hospitals overnight, which still seems unlikely to happen).
 5) “You can’t pour from an empty cup.”
5) “You can’t pour from an empty cup.”
6) #5 This applies to our mental health too — I worry this is just the beginning:
If it’s not too soon to say, what happens to us after this is all over?
 Will frontline healthcare workers be thrown back under the bus again? Will ERs still be used for med refills and work notes thereby continuing an increase of exposure to hospital-acquired infections?
Will frontline healthcare workers be thrown back under the bus again? Will ERs still be used for med refills and work notes thereby continuing an increase of exposure to hospital-acquired infections?
 How will we pay off $200k in student loans after many of us get disabled or we’re too scared to go back to work after this pandemic? Will the public turn on us saying that we had overreacted and now we have too many beds/PPE/ventilators (which scenario I’d rather have than being left with too FEW ventilators and we’d instead be rationing medical care/deciding who lives and who dies)?
How will we pay off $200k in student loans after many of us get disabled or we’re too scared to go back to work after this pandemic? Will the public turn on us saying that we had overreacted and now we have too many beds/PPE/ventilators (which scenario I’d rather have than being left with too FEW ventilators and we’d instead be rationing medical care/deciding who lives and who dies)?
 What about the PTSD some of us will face after some of our colleagues have already died/went on life support/hospitalized/lost 20% of their lung function after having been intubated? How do we feel safe going back to work when another pandemic might be right around the corner? How will we know we’ll have enough PPE next time? Why did we some of us have to resort to personal donations for PPE?
What about the PTSD some of us will face after some of our colleagues have already died/went on life support/hospitalized/lost 20% of their lung function after having been intubated? How do we feel safe going back to work when another pandemic might be right around the corner? How will we know we’ll have enough PPE next time? Why did we some of us have to resort to personal donations for PPE?

What if the next pandemic is equally as contagious as COVID-19 (asymptomatic for up to 25 days) but be as lethal as Ebola? #justsayin
While I’m grateful for relative progress, I’m holding my breath for the worst that’s yet to come (as if the worst hasn’t already happened).
7) Until we get around to those questions, at least think about them and to the best of your ability (I understand if it’s getting too difficult…I’ll still go back into work and put out the fires), keep #stayingthefuckhome
For further immediate, live updates on the ground, follow the stories posted on my Instagram: https://www.instagram.com/monsoondiaries/
![]()

